Ovarian cancer remains one of the most formidable challenges in oncology, particularly due to its silent progression and late-stage diagnosis, which complicate treatment and significantly reduce survival rates. High-grade serous ovarian carcinoma (HGSOC) is the most prevalent and aggressive variant, wreaking havoc in those diagnosed. Despite years of research, understanding the origins of this cancer has been elusive, typically attributed to a lack of visible symptoms until advanced stages are reached. Recent research utilizing mouse models, however, has illuminated potential avenues for early detection and intervention, particularly focusing on the fallopian tubes—a site previously underestimated as a source of ovarian cancer.
For over a decade, accumulating evidence has suggested that many ovarian cancers arise not within the ovaries themselves, but instead in the fallopian tubes. Studies have identified genetic lesions at the distal ends of these tubes that correlate strongly with tumors found in the ovaries, proposing a different narrative about the cancer’s initiation. This shift in understanding is crucial; if confirmed in humans, it could revolutionize screening methods and lead to earlier detection of this deadly disease.
The groundbreaking investigation led by Dr. Alexander Nikitin of Cornell University has enhanced our knowledge of the distinct cellular makeup within the oviducts of mice, revealing specific cell types that may bear responsibility for the onset of HGSOC. By mapping these cell types, researchers have embarked on a path toward uncovering precise diagnostic markers that can aid in the identification of cancer at its nascent stages—offering perhaps the best hope for improving patient prognoses.
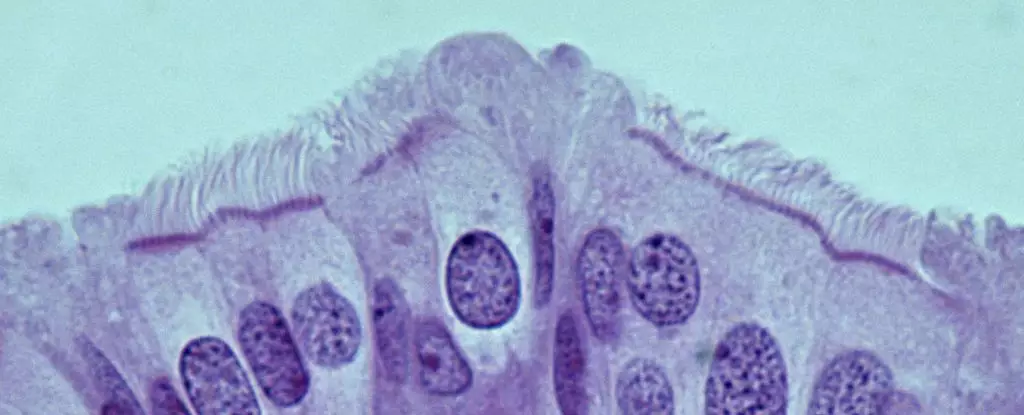
Previous research hinted at the existence of ovarian stem cells linked to HGSOC, but this new study unveils a more complex scenario. Dr. Nikitin’s team has identified that within the mouse oviducts, the cells displaying the highest propensity toward malignancy are not stem cells, as one might expect. Instead, it is the pre-ciliated cells—transitional cells that eventually develop into ciliated cells—that exhibit a striking vulnerability when subjected to specific genetic mutations. This discovery deviates from common assumptions and underscores the necessity of looking beyond conventional cell types when exploring cancer origins.
The significance of this finding is heightened by the realization that pre-ciliated cells play a vital role in facilitating the movement of oocytes through the oviduct. The mutations associated with HGSOC disrupt the normal functions of these pre-ciliated cells, leading to a cascade of events that promote cancer development. This realization not only deepens our understanding of the biology behind HGSOC but also points clinicians towards potential therapeutic interventions that could target these specific cell types and their disrupted functions.
Interestingly, the dysfunctions related to cilia—microscopic, hair-like structures on cells—have also been implicated in other cancers, such as pancreatic cancer. This connection between cilia and various malignancies suggests a broader biological theme that, if understood, could serve to enhance cancer prevention and treatment strategies across multiple types of the disease. Dr. Nikitin’s findings present a compelling case for further exploration into not just the genetic mutations driving HGSOC, but also the downstream effects these mutations have on cellular function in the fallopian tubes.
The implications of this research are profound. Should the cellular mechanisms identified in mouse models translate to human biology, we may soon see a transformative shift in how we screen for and treat ovarian cancers, particularly high-grade serous variants. The key next steps involve validating these findings in human tissues and elucidating the precise pathways leading from pre-ciliated cell dysregulation to cancer initiation.
While the journey toward a deeper understanding of ovarian cancer is far from over, the innovative research spearheaded by Dr. Nikitin and his colleagues represents a significant leap forward. The identification of cancer-prone cells within the fallopian tubes may lead not only to enhanced detection methods but also to the development of targeted therapies, offering hope to countless women battling this insidious disease.

Leave a Reply