For decades, neuroscience has viewed glycogen primarily as a standby energy reserve, a backup fuel stored in the liver and muscles, with little relevance to brain health beyond emergency scenarios. However, recent research challenges this reductive perspective, revealing that glycogen plays a far more complex and vital role within the brain, especially concerning neurodegenerative conditions like Alzheimer’s disease. A groundbreaking study from the Buck Institute for Research on Aging suggests that the way the brain manages its glycogen stores could be central to understanding, and ultimately treating, degenerative diseases marked by tau protein aggregation.
This shift in understanding is profound. Gone is the simplistic assumption that glycogen’s function in the brain is limited to temporary energy supply. Instead, the findings indicate that glycogen interacts directly with tau proteins, influencing the pathological trajectory of diseases characterized by tauopathy. This revelation prompts a reevaluation of how we approach neurodegeneration, emphasizing metabolic health and cellular chemistry as potential therapeutic targets. It underscores a paradigm where energy storage forms are not mere passive reserves but active players in disease progression.
The Intricate Relationship Between Glycogen and Tau Pathology
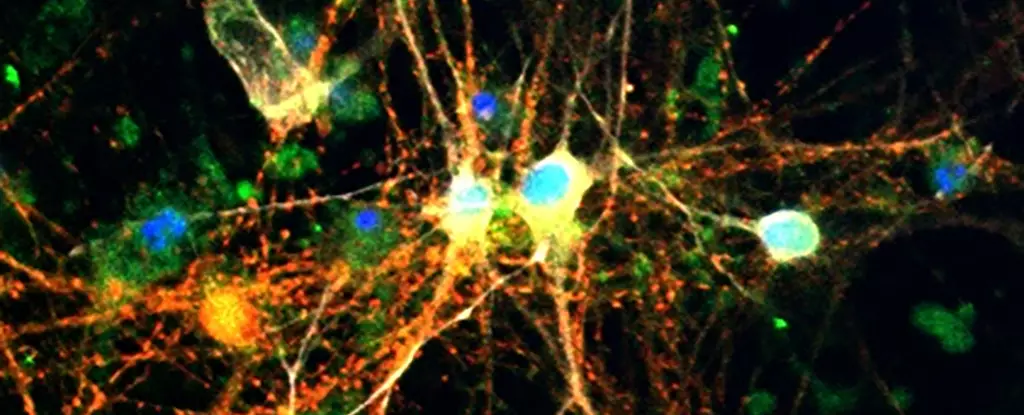
Delving into the research specifics, scientists observed abnormal glycogen accumulation not only in animal models of tauopathy—specifically, in genetically modified fruit flies—but also in the brains of humans diagnosed with Alzheimer’s disease. The critical insight is that tau proteins impair the brain’s ability to properly break down glycogen via the enzyme glycogen phosphorylase (GlyP). This impelled accumulation of glycogen, which compounds neuronal stress and dysfunction.
The consequences of disrupted glycogen metabolism extend beyond mere storage issues; they influence the cellular environment profoundly. Excess glycogen appears to facilitate a harmful interplay with tau, promoting neurodegeneration rather than protecting against it. Consequently, the presence of aberrant glycogen builds up alongside tau tangles, fracturing what was once thought to be a linear disease pathway into a more complex web of metabolic and biochemical interactions.
What stands out is the potential to intervene in this interaction. Enhancing GlyP activity in experimental models helped clear glycogen deposits, reduce oxidative stress, and limit neuronal damage. This suggests a new therapeutic window—boosting the brain’s ability to properly utilize glycogen could counteract one of the fundamental processes driving neurodegeneration. It’s a paradigm shift: instead of trying to remove tau or fix buildup later, what if we could prevent the cascade at its metabolic roots?
Diet, Drugs, and Future Therapeutics: A New Hope for Fighting Dementia
The most striking aspect of this research lies in its practical implications. If manipulating glycogen metabolism proves effective in animal models, it can open an entirely new frontier for treatments. The scientists experimented with dietary strategies – namely, implementing low-protein diets – showing that metabolic shifts could indeed prolong lifespan and reduce brain damage in affected flies. This aligns with existing evidence underscoring the benefits of caloric restriction and dietary modulation on brain health, but now with a molecular explanation rooted in glycogen management.
Furthermore, the team developed innovative pharmacological agents based on molecules like 8-Br-cAMP, which emulate the beneficial effects of dietary restriction by activating metabolic pathways that enhance GlyP activity. This preclinical success hints at future drug development targeting glycogen regulation, not just in flies but potentially in humans.
Adding to the therapeutic optimism is the link to existing drugs like GLP-1 receptor agonists – such as Ozempic – that are originally designed for diabetes management. These medications appear to influence glycogen pathways indirectly, providing a promising lead for repurposing existing pharmaceuticals to combat neurodegenerative diseases. Such strategies could offer more accessible, scalable treatments compared to experimental gene therapies or invasive procedures.
In essence, this emerging understanding positions glycogen metabolism as a promising target; one that bridges metabolic health and neuronal integrity. By harnessing the natural chemistry of sugar management within neurons, scientists are paving the way for innovative therapies that challenge outdated notions and focus on the systemic orchestration of cellular energy. In doing so, they offer hope that conditions like Alzheimer’s may one day be mitigated not just through symptomatic care, but by addressing core biochemical vulnerabilities.

Leave a Reply