The recent case of a severely ill elderly patient in Louisiana has alarmed health officials across the United States, marking the first critical human instance of avian influenza this year. This development comes amidst a growing tally of infections nationwide, which totals 61 confirmed cases as of now. The situation has escalated to the point that California, the most populous state in the country, has officially declared a state of emergency to bolster its response strategies. As countries globally brace for potential pandemics triggered by zoonotic diseases, the implications of these cases are far-reaching and merit urgent attention.
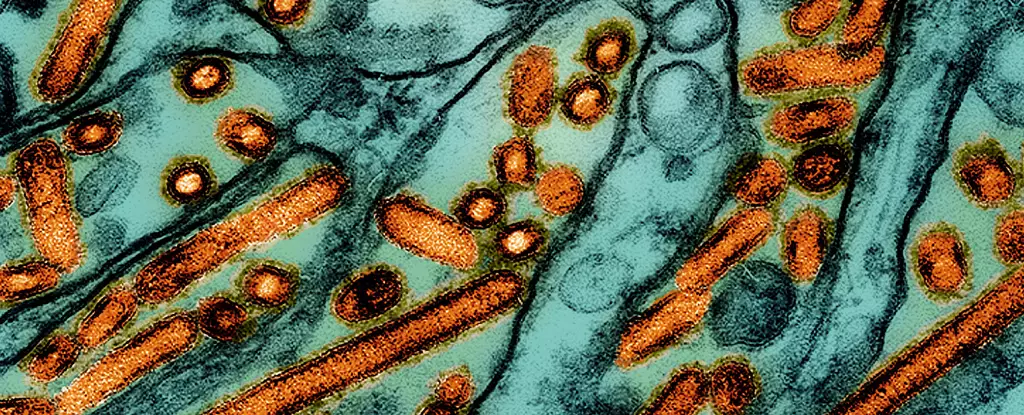
The strain of bird flu identified in the Louisiana patient is H5N1, notorious for its severe implications for both avian populations and human health. While most previous infections have shown mild symptoms, the critical condition of this elderly patient has drawn focus to the virus’s potential lethality. The Centers for Disease Control and Prevention (CDC) have noted that patients presenting symptoms similar to the Louisiana case often had a history of exposure to infected birds, underlining the need for enhanced biosurveillance in regions where avian species are prevalent.
Demetre Daskalakis, a senior official at the CDC, reinforced the urgency of understanding H5N1’s historical context — in some instances globally, up to 50% of patients afflicted with this variant have succumbed to the disease. The knowledge that this virus can cause severe outcomes in those infected emphasizes the necessity for coordinated federal efforts to manage its spread and protect public health.
In response to increasing concerns surrounding the avian flu outbreak, California’s state of emergency aims to ensure that agencies can mobilize resources effectively to counteract the threat. Governor Gavin Newsom’s proactive measures reflect a broader understanding of the public health landscape, spotlighting the need for accessible monitoring systems that swiftly identify potential avian influenza cases. This escalation suggests that local and state authorities are aware of the interconnectedness of agricultural health and public health, and underscores their commitment to protecting their communities.
Of note is that the identifying genetic sequencing of the H5N1 virus in the Louisiana patient suggests it belongs to the D1.1 genotype. This particular strain has been identified in both wildlife and poultry across the United States and has also been associated with severe incidents in other countries. The emergence of such genotypes raises questions regarding the adequacy of existing surveillance systems to accurately capture instances where animal-to-human transmission may either be undetected or more prevalent than currently estimated.
While experts emphasize the importance of maintaining vigilance, discrepancies in surveillance capabilities could hinder early detection of additional cases. The lack of a comprehensive understanding of the potential human-to-human transmission pathways, particularly under asymptomatic conditions, could create critical gaps in our preventative approach. The commentary from scientists like Laura Christofferson and epidemiologists highlights the potential reality that despite advanced preparation measures, being overly complacent could significantly jeopardize public health safety.
Public health organizations have already taken steps to prepare for possible scenarios of human transmission through stockpiling vaccines against H5N1. Recent research demonstrating the effectiveness of an experimental mRNA vaccine should provide a glimmer of hope, as it has shown promise in protecting ferrets from the virus. However, it becomes increasingly crucial to not only have vaccines in place but also to ensure rapid deployment and dissemination mechanisms are established for timely public health responses.
The emergence of avian influenza cases in the US raises questions beyond immediate medical concerns — including the potential risks presented by agricultural practices. The recent federal directives from the Department of Agriculture, mandating raw milk testing and reporting any positive cases of bird flu, illustrate the layered complexity of managing foodborne pathogens in conjunction with zoonotic diseases. This underscores the critical interdependence of animal health, food safety, and human well-being.
The avian flu situation serves as a stark reminder of the ongoing threat posed by emerging infectious diseases and the intricate interplay of ecological dynamics. As various stakeholders strategize on preventative measures, comprehensive interdisciplinary approaches that unify environmental health and public safety are paramount. As countries continue to monitor the situation, our collective response efforts must adapt swiftly to emerging data and trends, safeguarding public health in a globally connected environment.

Leave a Reply