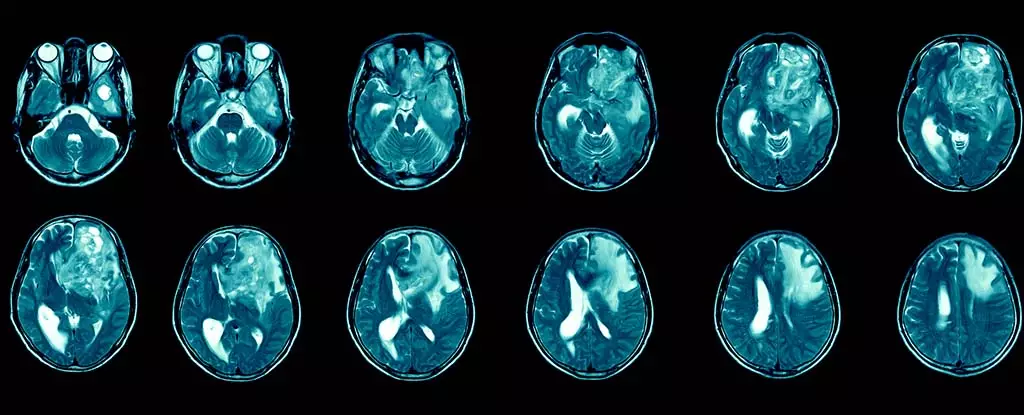
Glioblastoma multiforme (GBM) stands as a formidable adversary in the realm of oncology, often regarded as the most aggressive form of primary brain cancer. Defined by its rapid progression and intricate biological behavior, glioblastoma complicates treatment protocols for affected patients. Typically, the prognosis for individuals diagnosed with glioblastoma is disheartening. The average survival rate post-diagnosis hovers between 12 to 15 months, while only a mere 6.9% of patients manage to survive beyond five years. These statistics not only encapsulate the medical challenge posed by this malignancy but also reveal the emotional toll it inflicts on patients and their families.
Beyond mere survival statistics, glioblastoma manifests a host of debilitating symptoms that significantly deteriorate the quality of life for those afflicted. Patients often endure persistent headaches, seizures, and cognitive impairments, which can lead to profound personality changes. Such symptoms not only challenge day-to-day functioning but can also marginalize individuals in their personal and professional lives, raising urgent questions about effective therapeutic strategies.
Glioblastoma is classified as a grade IV tumor according to the World Health Organization, highlighting its aggressive nature. Each year, approximately 3,200 new glioblastoma cases are diagnosed in the UK alone, contributing to a total of around 12,700 brain and central nervous system tumors reported annually. When viewed from a global perspective, the incidence ranges approximately from 3.2 to 4.2 cases per 100,000 people, culminating in about 150,000 new cases worldwide each year.
One of glioblastoma’s main challenges lies in its remarkable resilience to standard treatments, which usually encompass surgical resection, radiation therapy, and conventional chemotherapy. These treatment modalities often yield temporary success due to the tumor’s ability to evade immune responses and the restrictive nature of the blood-brain barrier. Thus, even post-surgery, glioblastomas frequently recur, often metastasizing within the brain, which compounds the difficulties faced by healthcare providers in managing this aggressive disease.
In recent years, immunotherapy has emerged as a beacon of hope in the fight against various cancer types, including glioblastoma. This form of treatment aims to harness the body’s immune system to identify and eliminate cancer cells, presenting a paradigm shift from traditional approaches. Currently, immunotherapeutic strategies have shown success in managing other cancers, such as melanoma and lung cancer; however, their application to glioblastoma is still in the exploratory phase.
The nature of glioblastoma makes it inherently difficult to target with immunotherapeutic agents, as different tumor regions may harbor diverse genetic mutations. Nevertheless, researchers remain cautiously optimistic. Early trials indicate that specific immunotherapy techniques can be safely administered via injection into the cerebrospinal fluid, potentially paving the way for more effective penetration into these tumors.
Despite these advancements, the road to successful application of immunotherapy for glioblastoma remains fraught with obstacles. One significant challenge has been the chronic underfunding of brain cancer research, a situation that has hindered progress in identifying effective therapies. Fortunately, fresh initiatives are underway to engage multidisciplinary researchers, thereby enriching the field with new insights and perspectives.
For instance, I have spent over two decades studying the interplay between the immune system and cancer, with more recent work focusing on how immune cells interact with brain function akin to Alzheimer’s pathology. Applying this knowledge to glioblastoma research positions me at the forefront of a global initiative striving to develop more effective and targeted immunotherapy options.
It is crucial to underscore that as promising as immunotherapy may appear, it is not a universal remedy; not all cancers respond favorably to this approach, and the treatment comes with its own set of risks. Potential immune-related side effects, including organ inflammation, pose significant challenges. Careful administration is essential to mitigate risks, particularly when considering the potential for brain swelling.
The mode of delivery is another critical component in the quest for effective glioblastoma therapies. Preferably, non-invasive methods, such as peripheral injections or spinal administration, can significantly enhance patient comfort and safety compared to more intrusive surgical procedures.
Although glioblastoma remains a daunting challenge in oncology, immunotherapy holds the promise of revolutionizing treatment paradigms and improving patient outcomes. As interest and investment in this field continue to surge, there is genuine hope that innovative therapies will emerge to combat this devastating disease and enhance the lives of countless patients facing glioblastoma. With collaborative research efforts and continued advancements, we may soon witness significant breakthroughs in glioblastoma treatment, transforming despair into hope.

Leave a Reply