The menstrual cycle is often perceived as a natural biological rhythm impacting various aspects of life, primarily centered around reproductive health. However, recent research unveils an astonishing dimension: the complex interplay between hormonal fluctuations and structural changes in the brain. As neuroscientists delve deeper into this realm, there is a growing recognition that the impact of menstrual cycles extends beyond physical sensations and emotional changes, reaching into the very architecture of our neural networks.
Led by Elizabeth Rizor and Viktoriya Babenko at the University of California Santa Barbara, a team of researchers meticulously tracked the menstrual cycles of 30 women, focusing on the intricate relationship between hormonal levels and brain morphology. Their groundbreaking study is pivotal in that it sheds light on the concurrent changes in human white matter microstructure and cortical thickness influenced by hormonal rhythms throughout the menstrual cycle. Despite the frequency and ubiquity of menstrual cycles—around 450 periods over a typical lifespan—the scientific community has historically overlooked the neurophysiological implications.
The investigators highlight a notable deficiency in existing literature, stating that while previous studies have concentrated on cognitive performance during hormonal changes, little attention has been given to how these hormonal fluctuations shape the structural dynamics within the brain itself. By shining a light on this uncharted territory, Rizor and Babenko opened pathways for further exploration of how hormones orchestrate changes that may have far-reaching implications for behavioral health and cognitive function.
Hormonal Fluctuations and Brain Changes: The Findings
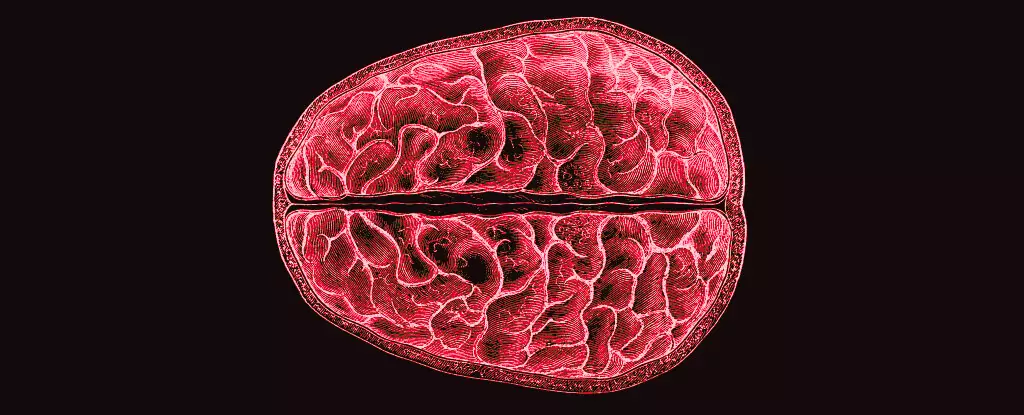
Utilizing MRI scans, the research team examined participants during three distinct phases of the menstrual cycle: menses, ovulation, and mid-luteal. This approach allowed for the observation of how varying levels of hormones relate to changes in brain structures, particularly focusing on white matter—a network that facilitates communication between different brain regions—along with gray matter, which processes information.
The findings were illuminating. As hormone levels shifted, significant changes in white matter microstructure and gray matter thickness were observed. Notably, the peak of 17β-estradiol and luteinizing hormone around ovulation was linked with adaptations in white matter that may enhance communication speed between brain regions. Additionally, fluctuations in follicle-stimulating hormone were associated with increased gray matter thickness, further indicating the complex ways these hormones influence structural brain changes.
The study also noted a fascinating connection between progesterone levels and tissue volume adjustments, which together with decreased cerebrospinal fluid volume, suggests a nuanced relationship between hormonal status and neural architecture. However, while the alterations observed provide crucial insights, the direct implications for cognitive processing and emotional regulation remain speculative—but ripe for future inquiry.
Understanding the multifaceted relationship between hormonal cycles and structural brain changes is essential, especially given the potential connections to mental health. Women have long reported mood fluctuations, cognitive variations, and even severe mental health concerns in relation to their menstrual cycles. The foundational insights garnered from this research could pave the way toward recognizing and addressing such issues, which have often been neglected in mainstream health discourse.
The implications stretch beyond mere awareness; they offer a framework for developing targeted interventions and support mechanisms for individuals experiencing menstrual-related mental health challenges. As researchers and healthcare providers deepen their understanding of these connections, individuals could be better equipped with knowledge and resources to navigate their experiences during different phases of their cycles.
The study led by Rizor and Babenko underscores the necessity of ongoing research into the effects of hormonal fluctuations on brain structure and function. As society grows increasingly aware of the importance of mental health, understanding how biological processes like menstrual cycles interweave with neurological health can inform better health practices and policies. By continuing to unravel the complexity of the menstrual cycle’s influence on the brain, we can empower individuals with knowledge and care strategies that are not only holistic but scientifically grounded.

Leave a Reply