Aging is often perceived as a straightforward journey characterized by declining health and an increase in various diseases, particularly cancer. However, emerging research presents a more nuanced picture that reveals a dual trend in cancer risk associated with age. Notably, while cancer risks escalate during the 60s and 70s due to the accumulation of genetic mutations, an intriguing drop in cancer risk has been observed in individuals over the age of 80. Recent studies are beginning to peel back the layers of this phenomenon, shedding light on the mechanistic underpinnings that might explain this counterintuitive trend.
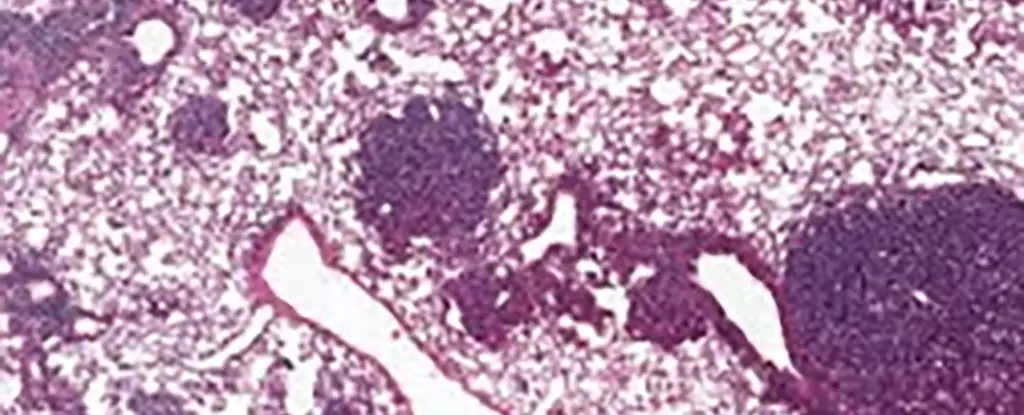
As individuals traverse through their later years, they often encounter a myriad of health challenges, with cancer being one of the most formidable. The cumulative effect of genetic mutations and environmental factors heightens cancer susceptibility in middle age. Yet, interestingly, research has suggested that by the time individuals reach their 80s, the risk may decline. One groundbreaking study conducted by an international team of scientists is exploring this dynamic, particularly focusing on lung cancer and a specific type of stem cell known as alveolar type 2 (AT2) cells.
At the heart of this inquiry lies a protein known as NUPR1. This protein is intricately linked to cellular behavior and appears to play a pivotal role in the aging process. What these scientists have observed is that older mice exhibit elevated levels of NUPR1, which inadvertently creates a scenario where cells functionally behave as if they are iron-deficient, even though they possess ample iron reserves. This paradoxical situation leads to a decrease in cellular regeneration and a limitation on both healthy growth and malignant tumor expansion, ultimately contributing to a lower cancer risk.
The relationship between iron metabolism and cancer is complex and has implications that extend beyond just aging. In young, healthy cells, iron plays an essential role in promoting growth and function. However, as the research suggests, the aging process alters this paradigm. Elevated levels of NUPR1 diminish the availability of iron to the cells, reducing their growth capabilities. When experiments demonstrated that suppressing NUPR1 or increasing iron levels reinstated cell growth, it became evident that targeting iron metabolism could offer new pathways for research into cancer treatments, particularly for older adults.
Importantly, the researchers also delved into the fascinating interplay between NUPR1 and a specific form of cell death known as ferroptosis, which is induced by iron toxicity. Their findings indicated that older cells exhibit a functional deficiency in iron that makes them less susceptible to ferroptosis, thereby presenting a potential barrier to effective treatment modalities based on this form of cell death. Understanding these mechanisms highlights the urgency of early intervention in cancer therapies, particularly those exploiting ferroptosis.
Furthermore, the insights gleaned from this research offer critical lessons in cancer prevention, particularly for younger populations. Experts emphasize that the carcinogenic risks associated with smoking, sun exposure, and other environmental factors during youth are more dangerous than previously understood. Targeted prevention in younger individuals could potentially mitigate their risk of developing cancer later in life, underscoring the importance of maintaining healthy habits from an early age.
A significant takeaway from the research is the necessity for personalized cancer treatment strategies. This study illustrates that treatment considerations must be attuned to a host of factors: the specific cancer type, its progression, existing health conditions, and importantly, the age of the patient. An age-informed approach could substantially enhance the efficacy of cancer treatments and lead to better health outcomes.
While aging presents a complex web of biological changes that interact intricately with cancer risk, ongoing research into proteins like NUPR1 and stem cell function holds promise. Understanding how these factors evolve with age may ultimately illuminate new pathways not only for cancer treatments but also for preventative strategies that enhance the quality of life for older adults. As we navigate the complexities of aging and cancer, continued inquiry is crucial to unraveling the many mysteries that still exist at the intersection of these two critical challenges.

Leave a Reply