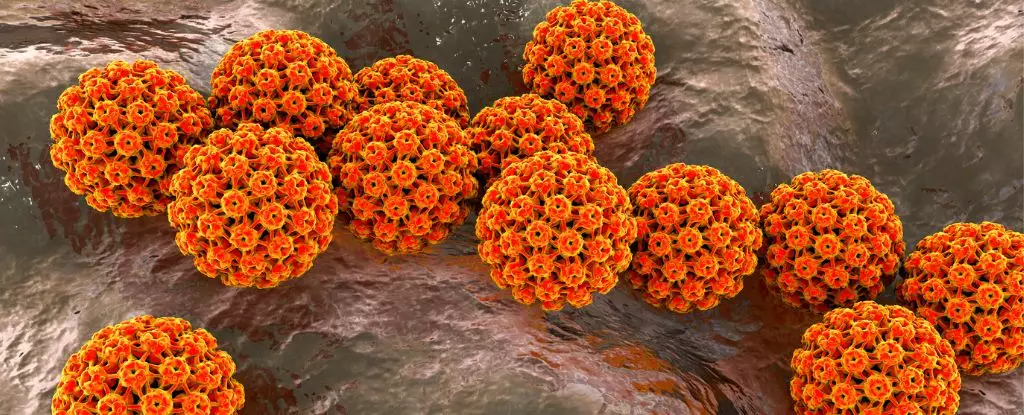
Recent research has revealed a pressing health concern: men are susceptible to contracting dangerous forms of oral human papillomavirus (HPV) throughout their lives. These findings are particularly alarming given the increasing incidence of oropharyngeal cancers, which affect the throat and mouth. This rise in cancer rates has been noted in various regions, especially in the U.S. and Europe, where men are diagnosed significantly more than women.
The need for heightened vaccination efforts emerges from the study’s findings. By focusing not only on younger males but also on middle-aged men—many of whom missed early vaccination opportunities—public health organizations have the potential to curb the formation of HPV-associated cancers. This is crucial since the surveillance data indicates a concerning epidemic of oropharyngeal cancers, primarily driven by HPV infections.
Human papillomavirus is a sexually transmitted infection recognized for its association with cancer. Different strains of HPV exist, but HPV-16 and HPV-18 are particularly notorious, contributing to nearly 90 percent of oral cancer cases. The significant takeaway from this research is the realization that risks associated with HPV do not diminish with age. Among a diverse group of over three thousand healthy men aged 18-70, researchers observed no decline in vulnerability to newly acquired cancer-causing strains of HPV as participants aged.
This perspective challenges preconceived notions that HPV primarily affects the young. With this understanding, it’s essential to reconsider the current vaccination recommendations, which have placed considerable emphasis on young individuals while overlooking older demographics who are also at risk.
Currently, vaccinations against HPV are recommended for individuals up to the age of 26 in the United States, yet rates at which young males receive this vaccine remain unsatisfactorily low compared to females. This discrepancy raises concerns about the potential rise in oropharyngeal cancer cases, even while cervical cancer rates have declined thanks to effective vaccination campaigns for women.
Recent calls from experts highlight the necessity of expanding vaccination programs to encompass older men, especially those who are immunocompromised or those with other cancer risk factors. There is a growing body of evidence suggesting that adults in their mid-lives could still gain substantial benefits from vaccinations, regardless of prior exposure to HPV strains.
A notable challenge in ongoing research efforts is the tendency of many studies to focus solely on males who engage in sexual activities with other males. This narrow view risks overlooking other pathways through which HPV can be contracted, including oral sex and skin-to-skin contact. As this study has indicated, the transmission dynamics of HPV are more complex, and taking a broader approach to survey different male populations is crucial.
Furthermore, the methodology of the current study—collecting oral gargle samples over multiple years—presents a more thorough analysis of the prevalence of oral HPV among men. Findings showed nearly 20 percent of participants already had prevalent infections, with about 6 percent carrying cancer-causing strains.
Anna Giuliano, an epidemiologist involved in the research, emphasizes the pressing need for continued awareness and tailored vaccination strategies. The extensive data pointing to consistent HPV acquisition across various age groups, combined with significant regional prevalence variations, underscores the urgency for public health initiatives to adapt.
It is clear that a unified, comprehensive approach towards HPV vaccinations is essential not just for young men, but for those at all ages. By fostering awareness and implementing more inclusive vaccination strategies, public health experts can effectively combat the rising threat of HPV-related oropharyngeal cancers—ensuring better health for future generations. The evidence is definitive: action is necessary, and the time to act is now.
Leave a Reply