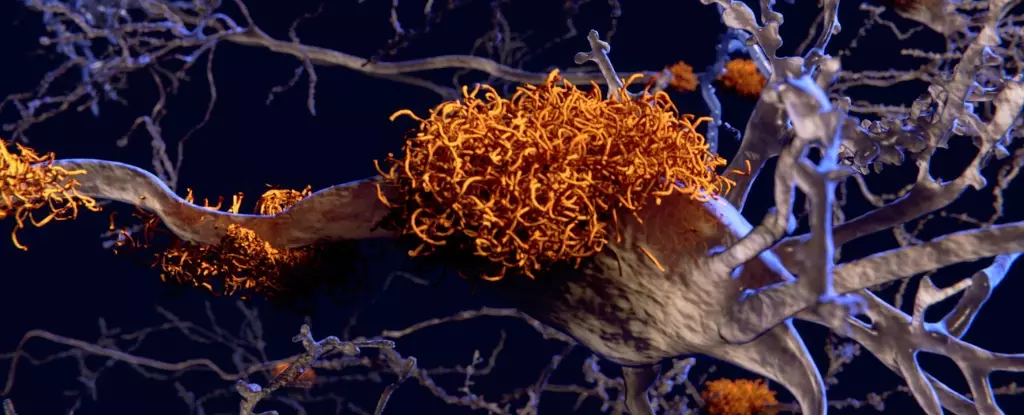
Alzheimer’s disease, a devastating neurodegenerative condition, has long been a topic of research and investigation. Recently, the role of the gut microbiome in the development of Alzheimer’s has garnered attention, with evidence suggesting a potential link. A study conducted by an international team of researchers has provided confirmation that the gut microbiota plays a causal role in the progression of Alzheimer’s disease. This breakthrough finding opens up new possibilities for understanding the disease and developing targeted therapies.
The study conducted by neuroscientists from University College Cork (UCC) in Ireland, King’s College London (KCL), and the IRCCS Saint John of God Clinical Research Centre of Bresci in Italy aimed to investigate the impact of the gut microbiota on brain health and behavior in Alzheimer’s patients. The research involved human participants, including individuals diagnosed with Alzheimer’s disease and healthy controls. Blood and stool samples were obtained from the participants to analyze the gut microbiota.
To further understand the causal relationship between the gut microbiome and Alzheimer’s disease, the researchers performed gut microbiota transplants on young adult rats. These rats had their microbiomes depleted by antibiotics and received transplants from either Alzheimer’s patients or healthy individuals. The rats were then subjected to behavioral tests to assess memory performance and other Alzheimer’s-related traits.
The results of the study showed that rats receiving gut microbiota from Alzheimer’s patients displayed impaired memory behaviors, particularly in tasks that rely on adult hippocampal neurogenesis. The hippocampus, a region critical for memory and mood regulation, is one of the first areas affected by Alzheimer’s disease. Furthermore, rats with gut microbiota from Alzheimer’s patients showed more severe impairments in hippocampal neurogenesis when the donors themselves had lower cognitive test scores.
The researchers also observed significant modifications in the rats’ hippocampal metabolome, which consists of metabolites involved in cell maintenance, growth, and normal function. These changes may contribute to the reduced growth of new neurons in the hippocampus, further impairing memory formation. Although assessing hippocampal neurogenesis in living humans is challenging, the study demonstrated that blood from Alzheimer’s patients decreased neurogenesis in human neural stem cells in laboratory settings.
Moreover, the study found a correlation between gene expression in stem cells exposed to blood from Alzheimer’s patients and their cognitive test performance. This relationship was also associated with the types of bacteria present in their gut microbiota. Notably, Alzheimer’s patients had lower levels of bacteria from the Coprococcus genus, which are typically associated with healthy aging. Conversely, they had higher levels of bacteria from the Desulfovibrio genus, consistent with previous findings in animal models of Alzheimer’s and Parkinson’s disease.
The confirmation of the role of the gut microbiome in causing Alzheimer’s disease has significant implications for future research and therapies. Traditional therapeutic approaches often focus on treating cognitive symptoms after diagnosis, which may be too late to halt or reverse disease progression effectively. However, by understanding the role of gut microbes during the early stages of dementia, researchers can explore new avenues for therapy development and personalized interventions.
Future studies must take into account various factors that can influence gut microbiota, such as overall health status, lifestyle, and medication history. This comprehensive investigation will provide a more nuanced understanding of the complex relationship between the gut microbiome, cognitive decline, and Alzheimer’s disease.
The groundbreaking study on the role of the gut microbiome in Alzheimer’s disease has solidified its significance in disease development. The findings support the idea that specific bacteria present in the gut are directly linked to cognitive decline in Alzheimer’s patients. This research opens up promising opportunities for developing targeted therapies and interventions that may slow down or prevent the progression of Alzheimer’s disease. By focusing on the gut microbiome, scientists have unlocked new pathways for understanding and potentially treating this devastating neurodegenerative condition.
Leave a Reply