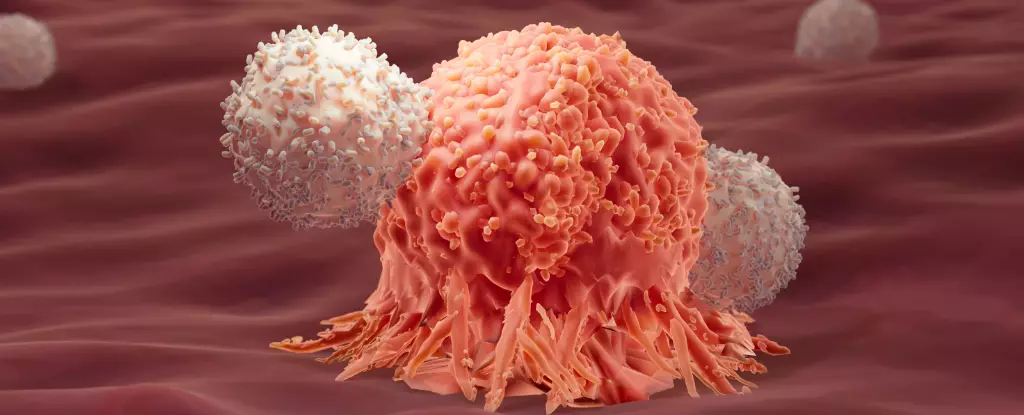
In recent years, immunotherapy has emerged as a promising avenue in the fight against cancer. By leveraging the body’s own immune system, researchers have sought to enhance the ability to recognize and attack malignant cells. This approach is particularly significant given the complexities surrounding cancer, which often evades conventional treatment methods. While immunotherapy has shown remarkable results in certain cancers, enduring success still remains elusive for many patients. Recent studies have pointed towards an unexpected solution—harnessing both the Yin and Yang of immune responses to potentially improve outcomes for cancer patients.
Traditionally, the immune system is understood through two primary response types: Type 1, primarily focused on targeting intracellular threats like viruses and cancer cells, and Type 2, which responds to larger pathogens such as parasites. Interestingly, the latter response has been traditionally viewed as counterproductive in the context of cancer; it was commonly believed that Type 2 responses may promote tumor growth rather than suppress it. However, new research suggests that this relationship might not be so straightforward. The interplay of these immune responses could create a synergy that offers new insights into how cancer therapies can be enhanced.
Researchers at École Polytechnique Fédérale de Lausanne (EPFL) turned their attention to patients with leukemia who had experienced lengthy remissions—some exceeding eight years—after undergoing CAR-T cell therapy. What they discovered was a significant presence of Type 2 immune markers among these long-term survivors. This revelation opens the door to a re-evaluation of the role of immune responses in cancer immunotherapy and suggests that a combined approach could yield more effective treatments.
To further delve into this intriguing correlation between Type 2 immunity and lasting remission, subsequent studies were conducted using animal models. Mice with colon adenocarcinoma were subjected to CAR-T cell therapy that utilized either a single Type 1 immune response or a combination of Type 1 and Type 2 responses. The results were striking—while all mice receiving only a Type 1 response succumbed to their tumors, 86% of those treated with the dual-response therapy exhibited complete remission.
These results lay the groundwork for a more nuanced understanding of immune interaction in cancer treatment. The combination therapy not only demonstrated a higher survival rate but also underscored how Type 2 immune responses, which were initially deemed irrelevant, could play a pivotal role in bolstering Type 1 responses against malignancies.
Closer examination of the modified immune proteins utilized in this dual approach revealed a connection to enhanced glycolysis—a critical metabolic pathway that supplies T cells with the necessary energy to effectively combat tumors. This energy boost appears to mitigate the exhaustion that often plagues immune cells during prolonged fights against cancer, thus enabling them to maintain their effectiveness over time. Such findings underscore the potential for refined immunotherapy strategies to integrate diverse immune mechanisms, ultimately leading to improved patient outcomes.
The compelling evidence linking dual immune responses with improved cancer treatment outcomes raises important questions about future directions in immunotherapy research. Could strategically combining Type 1 and Type 2 responses represent the next frontier in the development of cancer therapies? Researchers advocate for more extensive investigations into the nuances of immune interactions, stressing that while their findings establish a correlation, further studies are essential to truly understand the causal mechanisms at play.
The revelations from these studies herald a possible paradigm shift in cancer immunotherapy. By embracing the duality of the immune responses and exploring their synergistic potential, scientists can refine treatment strategies to better target resilient cancers. This approach not only shines a light on the complexity of the immune system but also fuels hope for patients seeking effective long-term solutions in the battle against cancer. As research progresses, patients, healthcare providers, and scientists alike await the practical applications of these findings in clinical settings, with the prospect of transforming cancer care on the horizon.
Leave a Reply